
Mental health awareness is an issue regularly reported in the media. There is no one cause of mental illness and often the cause is unclear. It can be the result of many events such as suffering caused from losing a loved one, diagnosis of terminal illness, the loss of a home, job or a multitude of challenges that people face daily, but sometimes it cannot even be pinned to a series of events or situations.
One area that can have an impact on mental health is our diet choices. By having an awareness of what certain food types do to our digestive system, we can be selective to ensure our food choices do not contribute to any mental health symptoms we are experiencing.

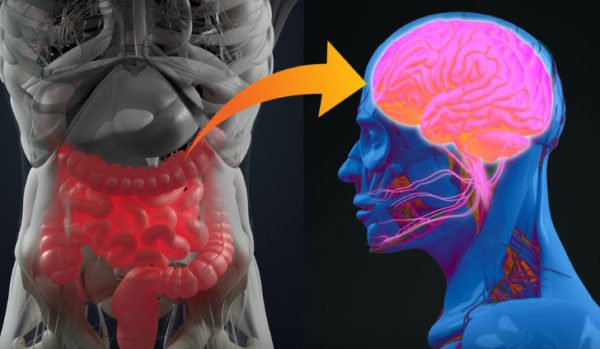
The Gut-Brain connection
Connecting the gut and brain to mental health is a new and fascinating area of research.
The gut-brain connection is now recognised as a basic tenet of physiology and medicine. There is no shortage of evidence of gastrointestinal involvement in a variety of neurological diseases. What has been discovered is that gut bacteria can play a significant role in psychology and behaviour as well as digestion.
The gut and brain are created from the same type of tissue. And so, intestinal health can have a profound influence on mental health, and vice versa. As a single system, the gut and brain work together to keep body functions operating at peak condition. They use the same methods and nerves to communicate. Hence, diet plays a huge role in mental health once we learn that the gut can be perceived as our “second brain”.
The gut has the same neurotransmitters and just as many neurons as the spinal cord and peripheral nerves. It contains almost 95% of a body’s serotonin, the neurotransmitter that helps regulate mood and social behaviour, appetite and digestion, sleep, memory, and sexual desire and function. Nourishing your gut flora is extremely important.
According to the World Health Organization, more than 264 million people of all ages suffer from depression. It is one of the leading causes of disability worldwide and a major contributor to the global burden of disease.
Dr. Michael Greger explains that the relationship between mental health and gut inflammation was first noted in 1887. The doctor who discovered this relationship was Julius Wager-Jauregg, the only psychiatrist to have ever won the Nobel Prize. There have been subsequent studies confirming this.
Fighting inflammation with plant-based nutrition

The modern diet is pro-inflammatory. This inflammation directly irritates the vagus nerve, the direct connection between the gut and the brain. The resulting mechanism has been detailed in many studies, including the Journal of Neuroscience Research, and the outcomes are the same. Our gut biome (the colonies of microorganisms that live in the gut) can be contaminated by the food we eat. The prime culprits are found in the modern mainstream diet.
The foods which most exacerbate inflammation are those that are mostly present in processed foods. These include simple sugars, fructose, dairy foods, eggs, alcohol, meat, hydrogenated fats, palm oil and some fruits and vegetables such as tomato and pineapple. These foods are not only causal in disrupting the gut biome but, if there is any inflammation in the body, they can feed the process.
Using data from two large studies, Danish researchers have found that higher blood levels of C-reactive protein (CRP) are associated with a greater risk of psychological stress and clinical depression. Eating a diet with significant amounts or animal protein can cause a burst of inflammation that could increase symptoms in someone already suffering from depression. Eating a diet rich in antioxidants, a plant-based diet, has a profound benefit in stress reduction.
This is good news since the gut biome changes with your diet. A plant-based diet can cut the C-reactive protein by 30% within two weeks because of the anti-inflammatory properties of antioxidants. This is important as clinical depression can be accompanied by increased oxidative stress and the autoimmune inflammatory responses it creates. Luckily, eating healthy is now easier than ever since there are a lot of sites that offer healthy meals ready to be eaten, an example of this is Proper Good.
Fermented Foods – the best route to optimal digestive health

Fermentation is a process that involves the breakdown of sugars by bacteria and yeast.
Fermented foods have been traditional staples in most cultures, but modern food manufacturing has eliminated most of these foods. You can find traditionally fermented foods like miso soup, tempeh, naturally fermented soy sauce or sauerkraut to feed your gut biome.
Going vegan has multiple proven benefits. An exclusively plant-based diet is naturally higher in fibre and boosts bacteria that make short-chain fatty acids (SCFAs). These SCFAs improve immunity against pathogens, provide an energy source for our gut lining, maintain the blood-brain barrier, activate critical intestinal protection mechanisms and help control our blood sugar and caloric intake.
Eat well and stay healthy.
By: Marlene Watson-Tara
Marlene Watson- Tara is the author of Go Vegan and co-founder of the Human Ecology Project. Here she writes about the significance of diet on a person’s mental state.
